Understanding Monkeypox: A Comprehensive Overview
Monkeypox is a viral disease that closely resembles smallpox, albeit less severe. Caused by the monkeypox virus, a member of the Orthopoxvirus genus in the family Poxviridae, this zoonosis can occur in certain animals and humans. This article provides a detailed understanding of monkeypox by exploring its history, transmission, symptoms, diagnosis, treatment, prevention, and impacts on public health.
Historical Context of Monkeypox
Monkeypox was first discovered in 1958 when two outbreaks occurred in colonies of monkeys kept for research, leading to its naming. However, the first human case was recorded in 1970 in the Democratic Republic of Congo (DRC), during a period when smallpox was being eradicated. Since then, monkeypox infections have been reported in several other central and western African countries, with occasional outbreaks outside of Africa largely attributed to international travel or animal importations.
Transmission and Spread
Monkeypox is primarily transmitted to humans through close contact with an infected animal’s blood, body fluids, or cutaneous or mucosal lesions. Human-to-human transmission, although less common, can happen through respiratory droplets during prolonged face-to-face contact, or by contact with infected bodily fluids and contaminated items such as bedding.
Bushmeat consumption and handling of infected animals are significant risk factors for zoonotic transmission. Forest-dwelling rodents and non-human primates like monkeys may harbor the virus and can transmit it to people.
In recent years, with increased international travel and changes to ecosystems that bring humans closer to animal habitats where the virus is present, there have been more frequent outbreaks. The variant viral strains in outbreaks outside of Africa tend to be less severe than those found in regions where the virus is endemic.
Clinical Presentation of Monkeypox
Monkeypox begins with a prodromal phase characterized by fever, intense headache, lymphadenopathy (swelling of the lymph nodes), back pain, myalgia (muscle aches), and an overwhelming feeling of malaise. After the fever onset, the patient develops a rash that often starts on the face then spreads to other body parts.
The pox lesions go through different stages before healing completely; they start as macules (flat bases), progress to papules (raised bumps), vesicles (fluid-filled blisters), pustules (pus-filled), and finally crusts over before falling off. The illness typically lasts from 2 to 4 weeks.
Distinguishing monkeypox from other pox-like diseases such as chickenpox can be challenging due to similar presentations. However, one notable feature is the presence of lymphadenopathy during monkeypox which helps differentiate it from varicella (chickenpox).
Diagnosis and Treatment
Diagnostic evaluation for monkeypox includes PCR (polymerase chain reaction) testing which can detect monkeypox virus DNA. In addition, electron microscopy may visualize the virus particles in samples but is not as commonly used due to its lower specificity.
As there is no proven, safe treatment for monkeypox virus infection, management focuses on symptom relief and supportive care such as hydration and infection control. Secondary bacterial infections should be treated accordingly. Complications such as pneumonia may also require supportive treatment including antibiotics.
Vaccines used during the smallpox eradication program also provide cross-protection against monkeypox. Newer vaccines have been developed specifically for monkeypox and are recommended for healthcare workers at high risk of contracting the disease or during outbreaks as ring vaccination strategies among contacts of cases.
Prevention Strategies and Public Health Implications
Preventing monkeypox requires a multifaceted approach including surveillance systems to detect cases promptly; public education about reducing risks of exposure; and strategies for controlling the disease among animals by restricting trade and use of bushmeat from affected areas. Education should focus on practices such as frequent hand washing, using personal protective equipment while caring for infected individuals or animals.
Concurrent with preventive efforts is policy making that relates to infectious disease control across borders; urging international cooperation; and employing quarantine procedures for confirmed cases if necessary. Collaboration with wildlife associations can help monitor animal populations that could harbor the virus.
The widespread health implications include strain on healthcare systems especially in nations where resources are limited; psychological and societal impacts due to fear of infection; economic fallout from reduced tourism; strain on trade due to import/export restrictions; consequences for conservation; and stigmatization inflicted upon affected communities.
Notes
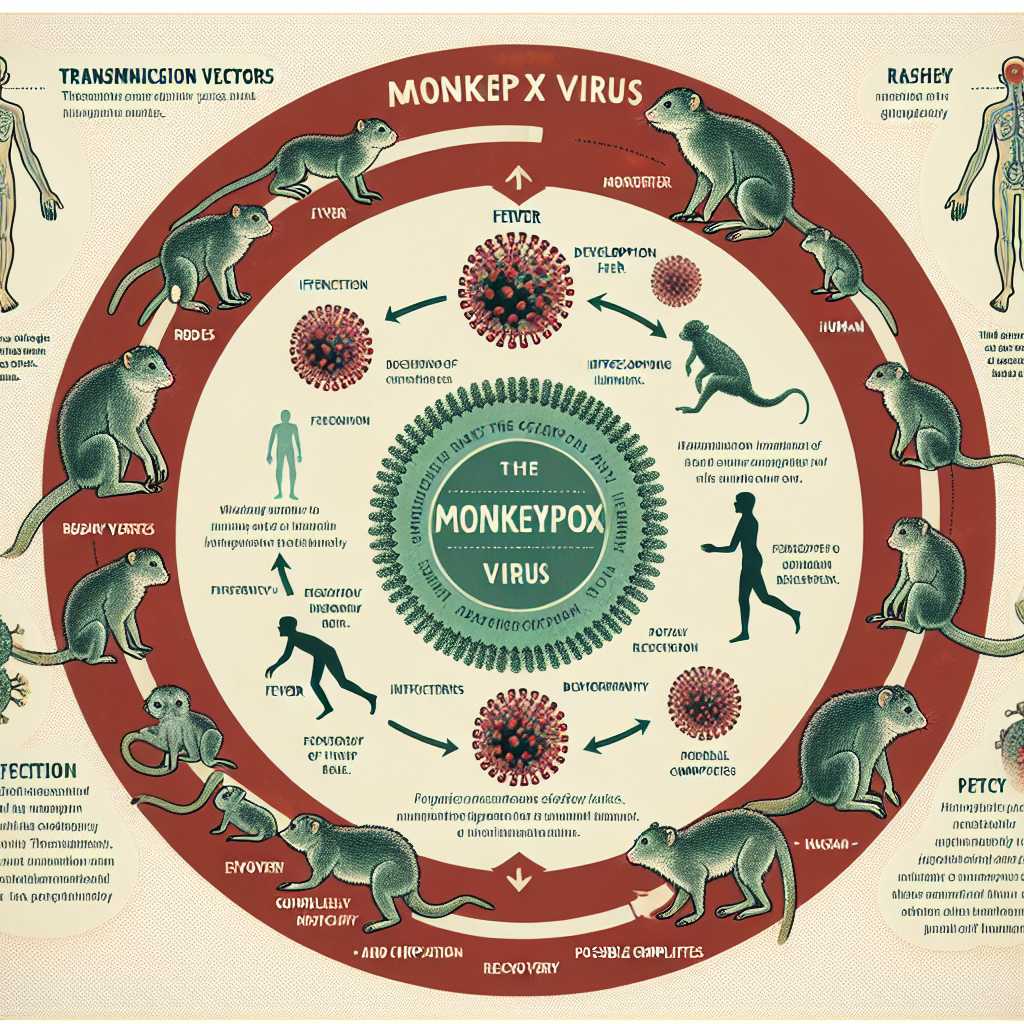
Image description: An informative graphic showing the Monkeypox virus lifecycle stages from transmission vectors (mostly rodents) to infection symptoms progression in humans starting from fever development through rash evolution until recovery or complication stages.