Understanding Graves’ Disease: An Overview of Causes, Symptoms, and Treatment Options
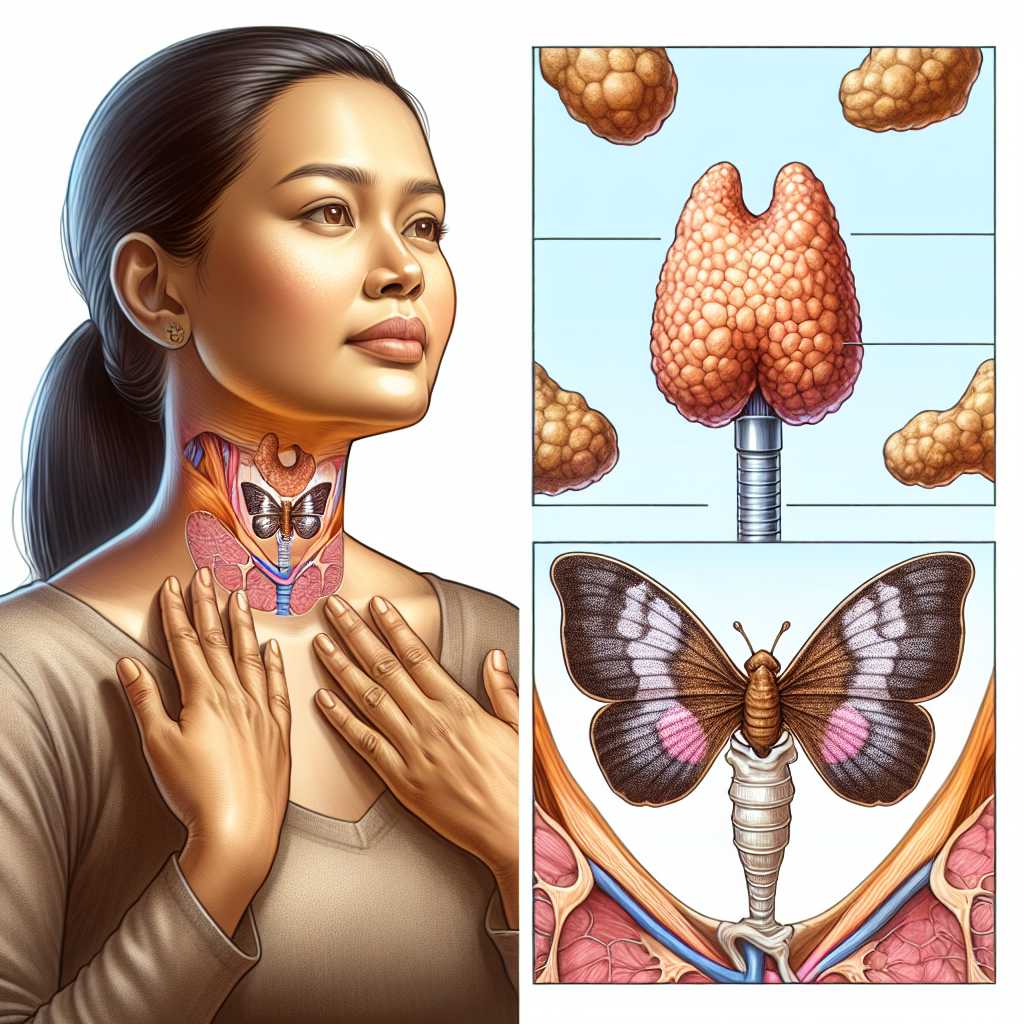
Graves’ disease is an autoimmune disorder that results in the overproduction of thyroid hormones (hyperthyroidism). This illness affects the thyroid gland, a butterfly-shaped organ located at the base of your neck, just below Adam’s apple. The thyroid plays a crucial role in regulating your body’s metabolism, affecting various body systems. Graves’ disease is the most common cause of hyperthyroidism and can have significant impacts if not managed properly.
The Pathophysiology of Graves’ Disease
Graves’ disease occurs when the immune system mistakenly attacks the thyroid gland. This interference causes the gland to produce more thyroid hormones than the body needs. This hyperactivity results in an acceleration of the body’s metabolism, leading to various health problems.
The exact reason why the immune system begins to target the thyroid cells remains unclear. Still, a combination of genetic and environmental factors is thought to play a role. Some researchers believe that a virus or bacterium might trigger the response in people genetically predisposed to the disease.
Recognizing the Symptoms of Graves’ Disease
The symptoms of Graves’ disease can be wide-ranging and affect different parts of the body:
– Weight loss despite normal eating habits
– Rapid or irregular heartbeat (palpitations)
– Increased appetite
– Anxiety and irritability
– Tremor of your hands or fingers
– Change in menstrual cycles
– Erectile dysfunction or reduced libido
– Frequent bowel movements or diarrhea
– Bulging eyes (Graves’ ophthalmopathy)
– Skin thickening and redness, typically on the shins and feet (Graves’ dermopathy)
It is important to note that not everyone with Graves’ disease will experience all these symptoms. Additionally, these symptoms can overlap with those of other conditions, making diagnosis based on symptoms alone challenging.
Diagnosis and Testing for Graves’ Disease
When Graves’ disease is suspected due to symptom presentation, several tests will be conducted for an accurate diagnosis:
1. Blood tests: Doctors check levels of thyroid-stimulating hormone (TSH) — and thyroxine. In Graves’ disease, TSH levels are typically low, whereas thyroxine (T4) levels are high.
2. Radioactive iodine uptake: A small, oral dose of radioactive iodine and an uptake test that measures how much iodine the thyroid collects from the bloodstream can indicate an overactive thyroid gland.
3. Thyroid scan: Used in conjunction with the uptake test, a scan allows doctors to visualize potential anomalies in the thyroid.
Current Treatments for Graves’ Disease
Multiple treatments are available for managing Graves’ disease. The treatment plan may depend on age, medical history, overall health, case severity, tolerance for specific medications or procedures, and patient preferences:
1. Anti-thyroid medications: Drugs such as methimazole (Tapazole) may be used to inhibit thyroid hormone production.
2. Radioactive iodine therapy: This treatment involves taking oral radioactive iodine to shrink the thyroid; however, it often results in hypothyroidism later on.
3. Beta blockers: These medications are usually used temporarily to ease symptoms.
4. Surgery (thyroidectomy): In some cases, where medication cannot be used, or in case of large goiters causing physical discomfort or difficulty breathing, surgery to remove part or all of the thyroid gland may be performed.
Post-treatment concerns generally involve managing hypothyroidism with lifelong throid hormone replacement therapy if the majority or all of the thyroid gland is destroyed or removed.
Complications Associated with Graves’ Disease
If left untreated or improperly managed, graves’ disease can result in complications such as heart-related woes (like rhythm disturbances), brittle bones (osteoporosis), pregnancy issues affecting both mother and fetus, and thyrotoxic crisis — a life-threatening condition needing urgent medical attention.
Living with Graves’ Disease
With proper medical care and self-management tactics like regular exercise, not smoking (to avoid aggravating eye conditions), addressing eye discomfort with lubricating eye drops or glasses that protect against wind and sun can improve outcomes significantly.
Prevention Strategies and Ongoing Research
There’s currently no proven way to prevent Graves’ disease since its cause largely remains mysterious. However, ongoing research into its pathogenesis may eventually reveal ways to interrupt its onset.
Notes
In summary, while Graves’ disease presents challenges such as varied symptomatology and potential long-term complications, its recognition has become better understood allowing efficacious treatment plans so that individuals affected can manage their condition effectively.
*Image description*: An illustration showing a person gently holding their hands around their throat area where the thyroid gland is located. Above it is an overlaid image of a healthy butterfly-shaped thyroid gland compared to a swollen one caused by Graves’ disease.