Understanding Cushing Syndrome: A Comprehensive Overview
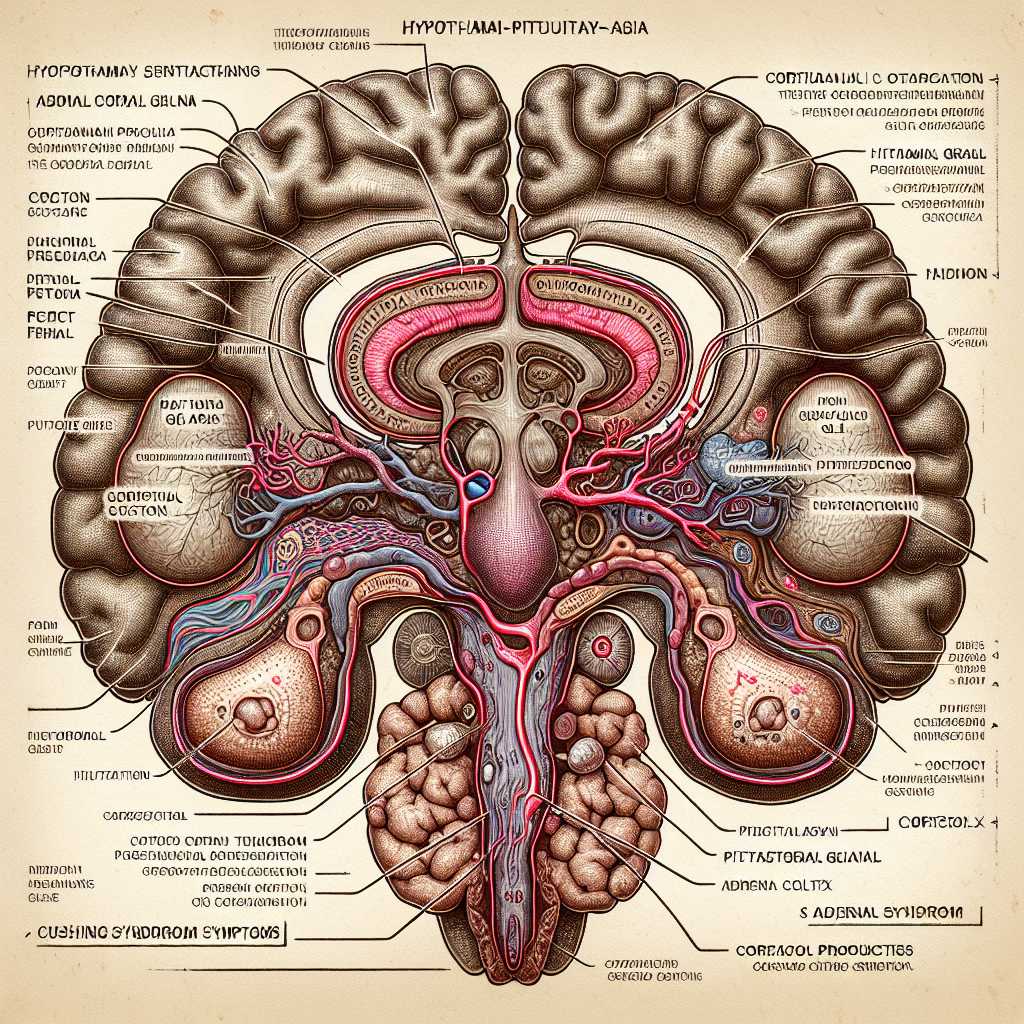
Cushing syndrome is a rare hormonal disorder characterized by prolonged exposure of the body’s tissues to high levels of the hormone cortisol. This condition can arise from various internal dysfunctions or prolonged use of corticosteroid medications. In this extensive article, we will explore the causes, symptoms, diagnosis, and treatment options, as well as the potential complications and outlook for individuals with Cushing syndrome.
Causes and Risk Factors of Cushing Syndrome
Cushing syndrome can develop from several causes that lead to excessive cortisol levels in the blood. Cortisol is indispensable for multiple functions including metabolism regulation, inflammation reduction, and assisting the body in responding to stress.
One primary endogenous cause is Cushing’s disease, where benign tumors called pituitary adenomas produce excess amounts of adrenocorticotropic hormone (ACTH), which in turn stimulates increased cortisol production from the adrenal glands. Non-pituitary tumors, such as those within the lung, pancreas, thyroid, or thymus gland, may also secrete ectopic ACTH leading to Cushing syndrome.
Further causes stem from the adrenal glands through development of nodules capable of producing cortisol independently of ACTH stimulation. These nodules may be benign or malignant in nature.
Most frequently though, the condition is attributed to exogenous causes. The long-term pharmacological administration of corticosteroids for conditions like asthma, rheumatoid arthritis, and lupus is often responsible.
Risk factors for developing this syndrome include demographic parameters; it is more common in adults aged between 20 and 50 years, and occurs more frequently in females than males.
Signs and Symptoms of Cushing Syndrome
The clinical manifestation of Cushing syndrome can cover a broad spectrum:
–
Physical signs typically include obesity centered around the abdomen. Patients may also notice a rounder face often described as a “moon face”, while accumulation of fat on the back of the neck and shoulders is outlined as a “buffalo hump”.
– Skin changes might include purple or pink stretch marks on the abdomen, thighs, arms, breasts, and shoulders. The skin itself becomes thin and fragile, leading to easy bruising.
– Musculoskeletal complaints see the muscle in arms and legs weakening while bones get more susceptible to fractures due to osteoporosis.
– Sexual health issues: Women may experience menstrual irregularities and hirsutism (excessive hair growth), whereas men might struggle with decreased libido or erectile dysfunction.
– Cognitive effects: Depression, anxiety, irritability and cognitive impairments are not uncommon.
– Other systemic effects: Hypertension, impaired glucose tolerance or diabetes mellitus, insomnia and headaches may all be related to elevated cortisol levels. Diagnostic Approaches for Cushing Syndrome
–
Skin changes might include purple or pink stretch marks on the abdomen, thighs, arms, breasts, and shoulders. The skin itself becomes thin and fragile, leading to easy bruising.
– Musculoskeletal complaints see the muscle in arms and legs weakening while bones get more susceptible to fractures due to osteoporosis.
– Sexual health issues: Women may experience menstrual irregularities and hirsutism (excessive hair growth), whereas men might struggle with decreased libido or erectile dysfunction.
– Cognitive effects: Depression, anxiety, irritability and cognitive impairments are not uncommon.
– Other systemic effects: Hypertension, impaired glucose tolerance or diabetes mellitus, insomnia and headaches may all be related to elevated cortisol levels. Diagnostic Approaches for Cushing Syndrome
–
Musculoskeletal complaints see the muscle in arms and legs weakening while bones get more susceptible to fractures due to osteoporosis.
– Sexual health issues: Women may experience menstrual irregularities and hirsutism (excessive hair growth), whereas men might struggle with decreased libido or erectile dysfunction.
– Cognitive effects: Depression, anxiety, irritability and cognitive impairments are not uncommon.
– Other systemic effects: Hypertension, impaired glucose tolerance or diabetes mellitus, insomnia and headaches may all be related to elevated cortisol levels. Diagnostic Approaches for Cushing Syndrome
–
Sexual health issues: Women may experience menstrual irregularities and hirsutism (excessive hair growth), whereas men might struggle with decreased libido or erectile dysfunction.
– Cognitive effects: Depression, anxiety, irritability and cognitive impairments are not uncommon.
– Other systemic effects: Hypertension, impaired glucose tolerance or diabetes mellitus, insomnia and headaches may all be related to elevated cortisol levels. Diagnostic Approaches for Cushing Syndrome
–
Cognitive effects: Depression, anxiety, irritability and cognitive impairments are not uncommon.
– Other systemic effects: Hypertension, impaired glucose tolerance or diabetes mellitus, insomnia and headaches may all be related to elevated cortisol levels. Diagnostic Approaches for Cushing Syndrome
–
Other systemic effects: Hypertension, impaired glucose tolerance or diabetes mellitus, insomnia and headaches may all be related to elevated cortisol levels. Diagnostic Approaches for Cushing Syndrome
Diagnostic Approaches for Cushing Syndrome
To diagnose Cushing syndrome accurately involves several steps:
–
Medical history and physical examination: A thorough recount of symptoms along with any medications taken is coupled with a physical exam looking for signs indicative of Cushing syndrome.
– Laboratory tests: These include urine tests (24-hour urinary free cortisol test), saliva tests for late-night cortisol levels, and blood tests to measure cortisol levels throughout the day vis-a-vis ACTH levels.
– Imaging tests: CT scans or MRI scans can detect abnormal growths on adrenal or pituitary glands which may be causing Cushing syndrome.
– Petrosal sinus sampling: This specialized procedure aimed mainly at differentiating between pituitary and ectopic sources of ACTH accumulation involves measuring ACTH from veins draining the pituitary gland. Treatment Options for those Affected by Cushing Syndrome
–
Laboratory tests: These include urine tests (24-hour urinary free cortisol test), saliva tests for late-night cortisol levels, and blood tests to measure cortisol levels throughout the day vis-a-vis ACTH levels.
– Imaging tests: CT scans or MRI scans can detect abnormal growths on adrenal or pituitary glands which may be causing Cushing syndrome.
– Petrosal sinus sampling: This specialized procedure aimed mainly at differentiating between pituitary and ectopic sources of ACTH accumulation involves measuring ACTH from veins draining the pituitary gland. Treatment Options for those Affected by Cushing Syndrome
–
Imaging tests: CT scans or MRI scans can detect abnormal growths on adrenal or pituitary glands which may be causing Cushing syndrome.
– Petrosal sinus sampling: This specialized procedure aimed mainly at differentiating between pituitary and ectopic sources of ACTH accumulation involves measuring ACTH from veins draining the pituitary gland. Treatment Options for those Affected by Cushing Syndrome
–
Petrosal sinus sampling: This specialized procedure aimed mainly at differentiating between pituitary and ectopic sources of ACTH accumulation involves measuring ACTH from veins draining the pituitary gland. Treatment Options for those Affected by Cushing Syndrome
Treatment Options for those Affected by Cushing Syndrome
Curing Cushing syndrome usually aims at reducing excess cortisol in the patient’s body:
–
Surgery: The first option lies in surgical removal of tumor that secretes ACTH or cortisol; this could be from pituitary gland or other tissues. Success rates for pituitary surgery are quite high when conducted by experienced surgeons.
– Radiation therapy: If surgery isn’t entirely successful or isn’t possible due to health reasons, radiotherapy might be prescribed particularly to address pituitary tumors.
– Medications: Medicinal treatments could involve drugs that block cortisol synthesis or manage specific symptoms such as mifepristone for glucose control.
– Adrenal gland suppression: Corticotropin-releasing hormone (CRH) antagonists can suppress ACTH production which lowers cortisol secretion.
– Replacement therapy : Addresses endocrine deficiencies that occur after removing adrenal glands.
–
Radiation therapy: If surgery isn’t entirely successful or isn’t possible due to health reasons, radiotherapy might be prescribed particularly to address pituitary tumors.
– Medications: Medicinal treatments could involve drugs that block cortisol synthesis or manage specific symptoms such as mifepristone for glucose control.
– Adrenal gland suppression: Corticotropin-releasing hormone (CRH) antagonists can suppress ACTH production which lowers cortisol secretion.
– Replacement therapy : Addresses endocrine deficiencies that occur after removing adrenal glands.
–
Medications: Medicinal treatments could involve drugs that block cortisol synthesis or manage specific symptoms such as mifepristone for glucose control.
– Adrenal gland suppression: Corticotropin-releasing hormone (CRH) antagonists can suppress ACTH production which lowers cortisol secretion.
– Replacement therapy : Addresses endocrine deficiencies that occur after removing adrenal glands.
–
Adrenal gland suppression: Corticotropin-releasing hormone (CRH) antagonists can suppress ACTH production which lowers cortisol secretion.
– Replacement therapy : Addresses endocrine deficiencies that occur after removing adrenal glands.
–
Replacement therapy : Addresses endocrine deficiencies that occur after removing adrenal glands.
Recovery from any surgical treatment relies significantly on early detection; therefore timely clinical intervention becomes paramount.
Potential Complications Associated with Cushing Syndrome
If left untreated, Cushing syndrome could lead to potentially life-threatening conditions due to chronic high levels of circulating cortisol. Common complications include:
– Type 2 diabetes
– Hypertension
– Bone loss (osteoporosis)
– Frequent infections
– Thromboembolic events like deep vein thrombosis
The condition’s comprehensive impact on one’s overall health makes monitoring necessary even after successful treatment due to possible recurrence or development of additional issues including cognitive impairments or recurring depressive disorders.
Managing Life with Cushing Syndrome
Living with Cushing syndrome demands a multidisciplinary health-care approach to manage its symptoms effectively. Attention must be given to both physical health parameters such as weight control, bone density preservation, blood pressure regulation furthermore overseeing emotional wellness through psychological support due to tendency towards mood swings or depressive conditions posed by enduring high cortisol challenges for extended periods.
Support groups can provide valuable personal experiences and relative assurance to those coping with this disorder, while adhering to therapy outcomes remains critical for extended term management.